Insight in the PhD of Anouk Scholten

An infant in an incubator within the neonatal intensive care unit (NICU) is a space of both fragility and risk. These vulnerable babies are faced with challenges that could profoundly shape their futures or may lead to fatality. With their entire lives ahead of them, these infants deserve the utmost in care. Research is thus very important.
Anouk Scholten performed her PhD research at the Neonatology department of the Emma Children’s Hospital, Amsterdam UMC. At this department critically ill term infants and preterm infants are admitted. As a technical physician her research was focused on cardiorespiratory monitoring based on the measurement of diaphragm activity using electromyography (dEMG). TMSi interviewed Anouk to learn more about the research that she performed together with the dEMG research team of the Neonatology department. The main research questions of her PhD research were: what is the clinical utility of dEMG in newborn infants and how can this technique be implemented in the clinical setting?
Hi Anouk, can you tell us why cardiorespiratory monitoring is so important?
Of course, at the NICU, critically ill term infants and preterm infants are admitted. Preterm infants have an immature respiratory system which often leads to an unstable breathing pattern with frequent breathing pauses (apnea) and a hampered lung function. These infants require monitoring of heart rate and breathing pattern (cardiorespiratory monitoring) to assess their clinical status and to detect critical events. When these events are early detected and treated, morbidity and mortality can be prevented. Therefore, cardiorespiratory monitoring is essential at the NICU.
How has cardiorespiratory monitoring been done?
Currently, cardiorespiratory monitoring is performed using electrocardiography (ECG) to assess heart rate and chest impedance (CI) to measure the respiratory rate. Chest impedance measures respiration indirectly via lung aeration and thoracic wall expansion. However, this technique has several disadvantages. One of them is susceptibility to cardiac muscle activity, which can be mistakenly detected as a respiration signal. Another disadvantage is sensitivity to movement; movement of the infant may produce a respiration signal during apnea. Both hamper reliable respiratory monitoring and the detection of apnea.
How could this be improved?
With diaphragm electromyography (dEMG) the activity of the main respiratory muscle, the diaphragm, is measured and thereby a direct insight into the respiration can be obtained. This technique provides insight in the heart rate, respiratory rate and breathing effort. Research conducted at Amsterdam UMC has demonstrated that this technique can be used for cardiorespiratory monitoring. Additionally, dEMG can be used to assess diaphragmatic function, and potentially to titrate and trigger respiratory support. At the Amsterdam UMC, a lot of research is performed on dEMG. Specifically, Anouk’s PhD research focused on exploring the clinical utility of dEMG and on how to implement this technique in a clinical setting.
What is the clinical setup you are using at the NICU?
Measuring diaphragm activity in infants can be performed invasively using a special naso- or orogastric catheter with embedded electrodes or noninvasively using transcutaneous EMG. Among others due to their vulnerability our research group uses transcutaneous EMG ofe diaphragm. To measure diaphragm activity through dEMG, three snap-on electrodes are used. Two of these electrodes are placed bilaterally in the midclavicular line at the costal margin, while the reference electrode is placed at the sternum. The dEMG signals are amplified using the Porti system of TMSi. Two unipolar derivations are made and subtracted to obtain a bipolar derivation, which is used as input for post-processing. The set-up can be seen in Figure 1.
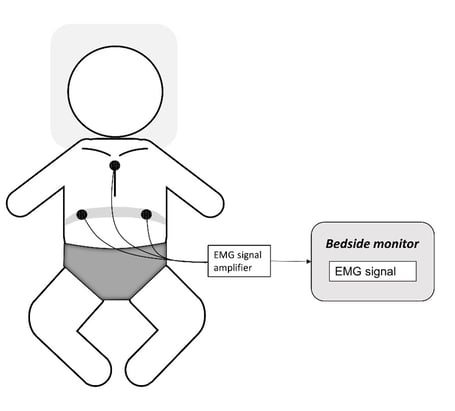
Figure 1: Measurement set-up for transcutaneous EMG of the diaphragm (dEMG). Two EMG electrodes are placed at the height of the diaphragm and one reference electrode is placed on the sternum. These electrodes are attached to the Porti of TMSi which is connected to a bedside monitor.
How do you analyze the data?
The raw dEMG data is analyzed by first removing the offset, drift, and cardiac activity. Afterwards, the signal is rectified and then a moving average or a root-mean-square can be calculated to obtain a respiratory waveform. Then, several EMG parameters can be calculated such as the peak activity and tonic activity (baseline activity). In addition, the respiratory rate can be calculated and the raw EMG signal can be used to determine the heart rate. All these steps can be seen in Figure 2.
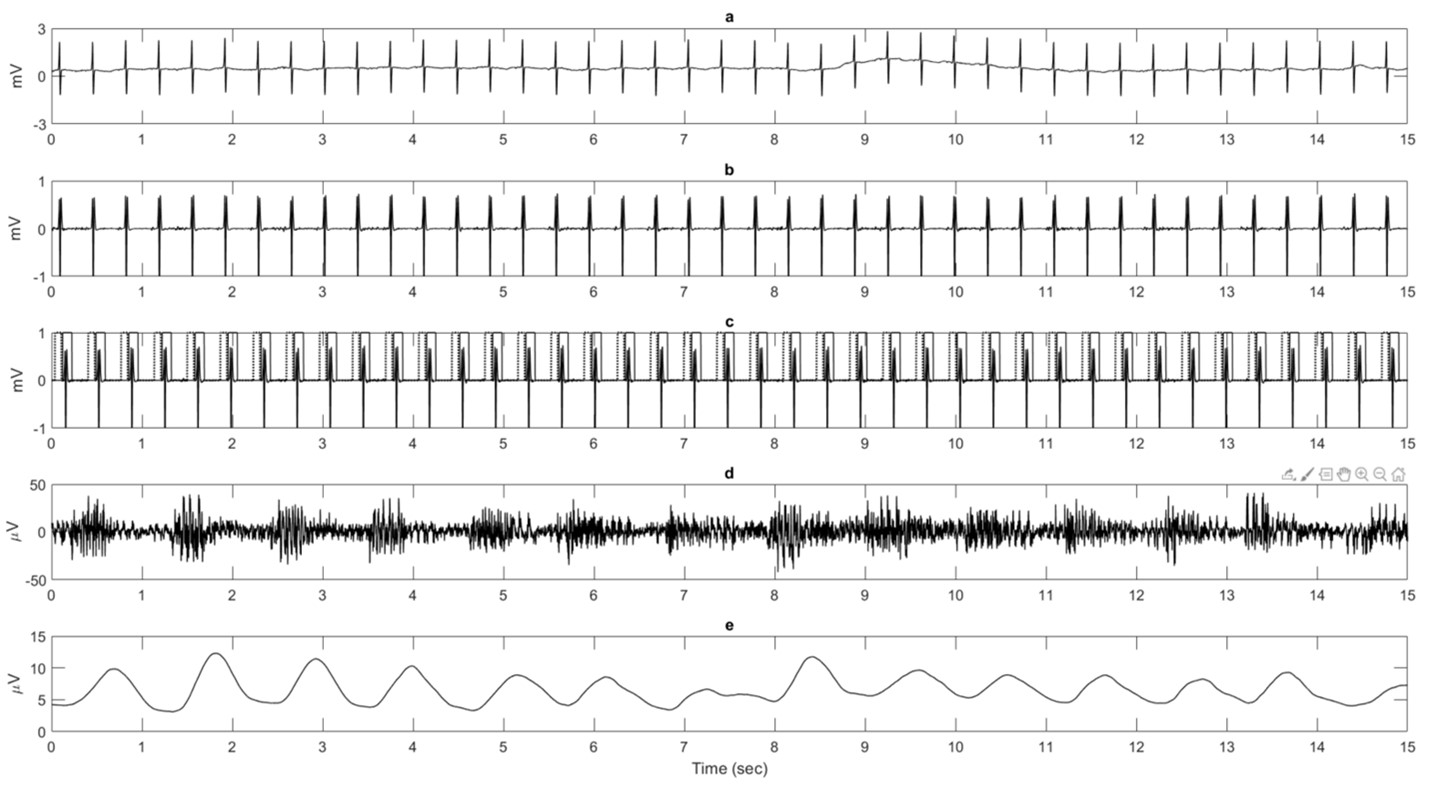
Figure 2: Illustration of signal analysis steps to generate a respiratory waveform starting with a raw diaphragm EMG (dEMG) signal using the transcutaneous technique (a). (b) The dEMG signal after filtering to remove the offset and drift. (c) Gates are placed around the detected QRS-complexes (solid line) and P-waves (dotted line). (d) The result after gating and filling the gaps with data. (e) The respiratory waveform after rectification and moving average filtering.
What are the challenges of using this method?
Unfortunately, dEMG measurements suffer from movement artifacts due to among others movement of the infant or during nursing care. This can result in that some of the data is less reliable.
What are the future prospects for this research?
The ultimate goal of this research line is to implement transcutaneous dEMG in the NICU to enable cardiorespiratory monitoring based on diaphragm activity in all admitted infants. However, there are still some remaining challenges before this could become reality.
We would like to thank Anouk Scholten for her contribution to improve healthcare for newborn infants and for the time to tell us about her research. If you would like to get to know Anouk better look at her LinkedIn page.